
After making the decisions around a breast cancer diagnosis, you have chosen a mastectomy and reconstruction. Understandably, you may still have some questions – not just about the procedure itself, but about what to expect afterward. One of the most common questions we get is: How much will it hurt?
Mastectomy is an operation that removes all of the breast tissue from one or both breasts. It is an effective weapon against breast cancer. However, in the process of removing the breast tissue, nerves and other tissues are also necessarily removed. In years past, it was not uncommon to experience significant postsurgical discomfort during the recovery period. A recent survey showed that patients’ number one concern leading up to surgery was pain. Uncontrolled, acute postoperative pain can lead to an increased surgical stress response which has effects on various organ systems. In addition, uncontrolled acute postoperative pain is associated with longer stays in the recovery room and hospital. Finally, as many as 30% of patients suffer chronic pain after mastectomy, and as such, effective acute pain control remains vital to patient recovery following breast cancer surgery.
Fortunately, recent developments have markedly improved the experience for our breast cancer and reconstruction patients. We now understand there is a role for treatments before, during, and after surgery to ensure a fast, comfortable, and smooth recovery. The before focuses on the new “enhanced recovery after surgery or ERAS” protocols (the subject of a future blog). During surgery, there are now nerve blocks that can be done to strikingly reduce discomfort after surgery and is the focus of today’s blog. By understanding and implementing these novel strategies before and during surgery, the after-surgery part almost takes care of itself. The vast majority of our patients use nothing more than Tylenol and ibuprofen to manage discomfort after surgery and here is how we accomplish that.
The classic postsurgical pain management protocol consists of narcotics (also called opioids or prescription painkillers). While narcotics are potent pain relievers, they can cause unwanted side effects such as drowsiness, itching, nausea, vomiting, constipation, and even difficulty breathing. Additionally, there is a small risk of addiction as seen in the recent opioid crisis in Arizona. The good news is that narcotic use can be minimized or even avoided entirely with ERAS and nerve blocks.
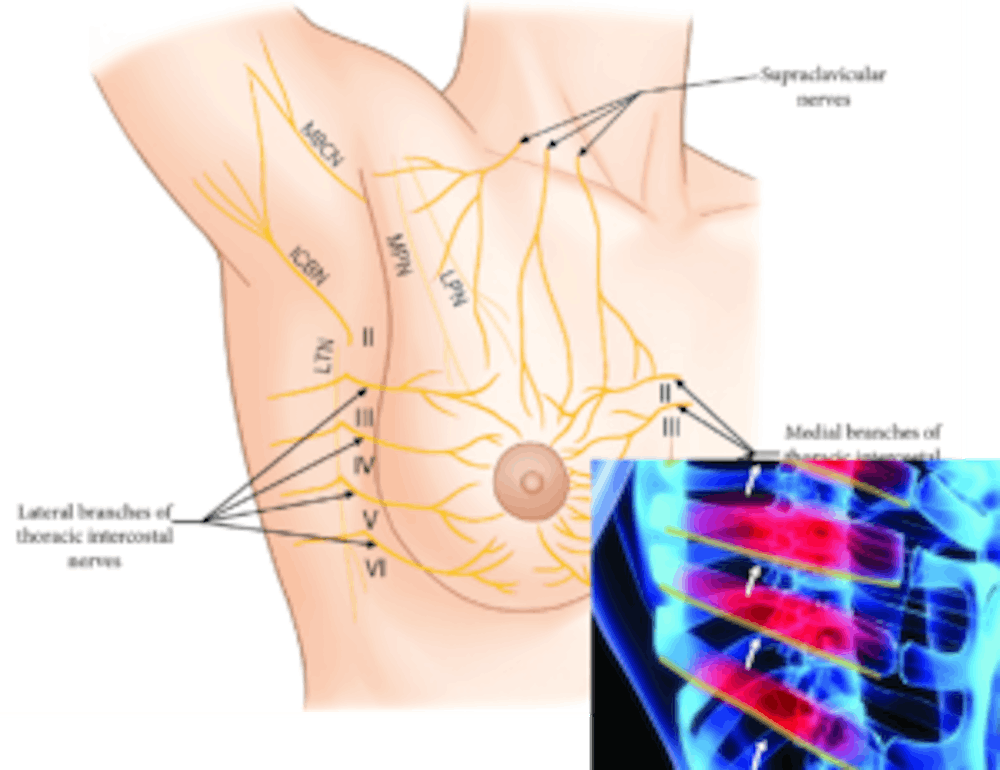
The feeling (sensation) of the breast comes mostly from the intercostal nerves located under each rib. With the patient asleep in surgery, a needle is used to inject local anesthetic just below the lower edge of the rib. This is then repeated at multiple levels. Next, local anesthetic is also injected as a “field” block where we inject local all around the breast to numb the other minor nerves supplying the breast. With that, we can essentially numb the entire area. Most local anesthetics last 4-6 hours at most. Drs. Mahabir and Kurtovic have advocated for patients and received special permission to use an innovative medication for their breast reconstruction patients: Exparel. Exparel contains a specially formulated bupivacaine (a type of local anesthetic) that is designed to release into the surgical site over a long period of time. Patients that receive this medication experience pain relief for 3-4 days!
***For our DIEP flap patients, a similar nerve block can also be performed in the abdomen: transversus abdominis plane block (TAP) block. Exparel is injected between different layers of the abdominal wall and blocks the nerves supplying the anterior abdomen. You too may use very little narcotics and combined with the Enhanced recovery protocol, you will be home one or two days after surgery and taking only over the counter medications.
Postsurgical pain would normally be at its worst for the 24 to 72 hours after surgery, so by using exparel, discomfort is minimized during this critical period ensuring a fast recovery and the patient’s long-term well-being. By using a combination of non-narcotic analgesics (pain medications) and the long-acting local anesthetic, we are able to get our patients through the most difficult portion of their recovery without putting them at risk for narcotic-related side effects.
Starting a dialogue with your surgeon can be as simple as asking “How will my pain be managed after surgery?” Don’t be afraid to ask! Many patients either take safe and adequate pain management for granted or are too overwhelmed with information and never broach the issue with their doctor. But by not initiating a discussion, you’re missing out on the opportunity to have a voice in choosing the types of pain treatments or medications you’ll be given.
Don’t wait until the day of your surgery to talk to your doctor about pain management, and don’t be afraid to express your preference to minimize the use of narcotics after surgery. You are your best advocate.

